-
Pre-Operative NPO Recommendations
Pre-Operative NPO Recommendations
NOTE: There are many medications patients should/should not take when NPO and awaiting surgery. For more specific instructions on medications prior to surgery, please refer to Perioperative Medication Management Recommendations. Staff should always follow surgeon/proceduralist directions if provided.
Simplified MINIMUM NPO guidelines: (excluding medications)
All Ages:
2 hoursfor clear liquids (CLEAR juices with no pulp, plain jello, black coffee, CLEAR sodas*)
4hoursforbreastmilk
6 hoursfor infantformula
8 hours for non-clear liquids andsolids** (includes non-human milk, hard candy and chewing tobacco)
Longer fasting times improve flexibility in moving cases up. When in doubt, follow surgeon instructions.
Anesthesia recommends Ensure Pre-Surgery as the clear carbohydrate drink of choice.
If Ensure Pre-Surgery not available or provided, an alternative 8oz CLEAR carbohydrate drink with NO PROTEIN such as a soda or Gatorade is encouraged no later than 2 hours prior to surgery unless contraindicated by surgeon (diabetic patients excluded).
Gastric tube feedings are considered solids.
-
Peri-operative Medication Management
Perioperative Medication Management Recommendations
NOTE: These recommendations from the Departments of Anesthesia and Perioperative Medicine are to serve as guidelines for physicians and their staff when providing education to patients regarding their medications prior to surgery. It is not intended to be all-inclusive nor supersede physician-specific instruction. If there are specific concerns related to a medication, clarification and discussion should occur between the surgeon, the patient and the anesthesia provider and should include the risks, benefits and alternatives to proceeding, rescheduling or cancelling the procedure.
1. Cardiovascular and Hypertensive Medication
Beta Blockers—continue through surgery
Alpha 2 Blockers (clonidine)—continue through surgery
Calcium Channel Blockers---continue through surgery
Diuretics—
a)HCTZ taken for HTN-Hold day of surgery
b)Furosemide, Bumetanide, other loop diuretics and spironolactone taken for CHF-take day of surgery ONLY if EF<40% (assuming recent Echo available)
c)Furosemide, Bumetanide, other loop diuretics given for other reason or EF>40%, hold day of surgery (assuming recent Echo available)
ACE/ARB and renin inhibitor (Aliskiren/Tekturna)— Do not take day of surgery
Non statin lipid agents, niacin, and fibric acid agents (gemfibrozil, fenofibrate) and ezetimibe (Zetia)—stop day prior to surgery
Statins—continue through surgery
Repatha (evolocumab)-continue through surgery, administration every 2 weeks
Ranexa (ranolazine)-can take day of surgery
2. Gastrointestinal Agents
H2 Blockers and PPIs—continue through surgery
3. Pulmonary Medication
Metered dose inhalers---continue through surgery
Theophylline—stop the night before surgery
Leukotriene Inhibitors (zileuton, zafirlukast, montelukast)—continue through surgery
4. Endocrine Medications
Glucocorticoids
a)Patients taking glucocorticoids < 3 weeks or daily dose prednisone equivalent < 5mg or taking chronic every other day therapy are unlikely to need stress doses, continue usual meds through surgery
b)Patient with daily dose > 5mg or treated with > 5mg/day for > 3 weeks in the past year need stress dosing.
c)See attached chart for steroid stress dosing (Table II)
Diabetic Medications
a)Hold sulfonylureas, metformin and other oral agents on day of surgery (if risk of hypotension or need IV contrast, hold metformin for 48 hours).
b)SGL T2 Inhibitors (dapagliflozin, empagliflozin, ertugliflozin) -- hold for 3 days prior to surgery (5 days for bariatric surgery)
c)Evening prior to surgery
i.BG > 120—give usual dose of long-acting PM insulin (Lantus, Detemir, NPH)
ii.BG < 120—give 50% of usual dose of long-acting PM insulin (Lantus, Detemir, NPH)
iii.Give bedtime sliding scale correction of short-acting insulin ONLY if BG>150 at bedtime
d)Day of Surgery
i.Give 50% dose of AM long-acting insulin (Lantus, Detemir, NPH) on the day of surgery
ii.Mixed dosage insulin (70/30, 75/25) severely reduce or avoid all together AM of surgery
iii.Insulin Pump—continue basal rate
iv.U500-hold for surgery and cover with short acting insulin, resume post op (in hospital) at 50% of previous dose. If used in hospital, use U500 pen to avoid dose problems
v.The following meds are ok for surgery-won’t cause hypoglycemia BUT hold for GI surgery if ileus expected or may cause nausea and vomiting. Ok to hold also.
GLP-1 receptor Agonist
Exenatide (Bydrueon, Byetta)
Lixisenatide (Aldyxin)
Liraglutide (Victoza)
Abliglutide (Tanzeum)
Dulaglutide (Trulicity)
Glargine-Lixisenatide(Soliqua)
Degludec-liraglutide(Xultophy)
Dipeptidyl Peptidase-4 Inhibitors
Sitagliptin (Januvia)
Saxagliptin (Ongliza)
Linagliptin (Tradjenta)
Alogliptin (Nesina)
Hormone Medications
a)Oral Contraceptives
i)Low risk surgery for VTE can continue
ii)Intermediate risk or high risk procedures consider stopping 4-6 weeks prior to surgery (will need alternative contraceptive and pre surgery pregnancy test)
b)Post-Menopausal Hormone Therapy
i)Low risk procedure for VTE can continue treatment
ii)Intermediate and high risk procedures can consider stopping 4-6 weeks prior to surgery
c)Thyroid Medication-continue to take
5. Medications Affecting Homeostasis
Antiplatelet Agents
a)Patient at high risk for CV event and low risk for complications if bleeding occurs—continue ASA (call surgeon if any questions)
b)Stop ASA 7 days prior to surgery where bleeding would be catastrophic (e.g. intracranial, spinal, urological procedures) or where patient is low risk for CV event
c)Avoid stopping dual antiplatelet therapy for Percutaneous Transluminal Coronary Angioplasty < 2 weeks, Bare Metal Stent < 3 months, Drug-Eluting Stent(DES) < 12 months. After this time continue ASA 81 mg and stop other agent. Current recommendations 2018 from ACC state SOME patients may stop dual antiplatelet therapy at 6 months if needed. Need to discuss with cardiology if considering stopping before one year of DES.
d)Stop Plavix(clopidogrel) x 7 days
e)Stop Effient(prasugrel) x 7 days
f)Stop Brilinta(ticagrelor) x 5 days
Other Antiplatelet Agents
a)Stop cilostazol(Pletal) x 5 days
b)Stop dipyridamole x 2 days
c)Stop Aggrenox (aspirin/dipyridamole) x 7 days
NSAID
a)Stop 7 days prior to surgery. In case of Celebrex (celecoxib), if needed can consider to continue through surgery as little effect on platelets (elevated CV mortality)
Anticoagulation
a)Follow anticoagulation bridging protocol if prescribed by surgeon, PCP or anticoagulation clinic.
b)Coumadin (warfarin)
INR > 3.0 STOP > to 6 days prior to surgery
INR 2.0 to 3.0 STOP 5 days prior to surgery
If any question, order preop PT/INR
c)Dabigatran
CRCL > 50 ml/min stop 2 days prior to surgery
CRCL < 50 ml/min stop 3 to 5 days prior to surgery
d)Rivaroxaban and apixaban—stop 2 days prior to surgery, only 1/3 renal cleared—consider additional time for severe renal disease
e)SPINAL OR EPIDURAL ANESTHESIA—hold Factor Xa inhibitors or Direct Thrombin Inhibitor 72 hours minimum before procedure. Refer to appendix pc494xf-- Management of Antithrombotic Therapy for Neuraxial and Peripheral Nerve Procedures for additional guidance.
6. Psychiatric Medications
TCA—continue through surgery
SSRIs—may affect platelet function, generally continue
Lithium and Valproate—continue through surgery
Antipsychotics—may increase QT, especially with volatile anesthetics, continue with care for volatile anesthetics and antibiotics
Psychostimulants—for ADHD- hold on day of surgery
Antianxiety Agents—continue through surgery
MAO-Is - hold 2 weeks prior to surgery
Muscle relaxants including baclofen and cyclobenzaprine (Flexeril)-continue throughout surgery.
Phentermine-used for weight loss. Stop 7 days before surgery
Phendimetrazine-Stop 7 days before surgery
7. Chronic Opioid Therapy
Continue through surgery
For patients on high dose narcotics, consider Pain Management consultation for management postoperatively
Suboxone (buprenorphine/naloxone)—hold greater than or equal to 5 days prior. DO NOT resume until 2-3 days after patient’s last opioid dose. Send pts to providers that are prescribers for instructions on hold/not hold
Contrave (naltrexone/bupropion)-Stop 72 hours before surgery
**Disulfiram (Antabuse)
-Stop 10 days before surgery
-May decrease effectiveness of analgesics/sedatives
Buprenorphine—Hold 24 hours prior to surgery
Naltrexone—Hold for 3 days for opioid addiction. Hold for 5 days for other dx, i.e. weight loss
8. Neurological Medications
Seizure medication—continue through surgery
Muscle relaxants-see under psych meds. Continue throughout surgery
Antiparkinson Medication
a)For Deep Brain Stimulator and Parkinson Meds
i.Oral medications should be stopped by 6pm the night before Stage 1(lead implantation) of the procedure.
ii.Extended release tablets should be stopped 24 hours prior to Stage 1 of the procedure.
iii.Patches should be removed 72 hours prior to Stage 1 of the procedure.
iv.For Stage 2 of the procedure, patients can continue their Parkinson medications as prescribed.
v.If DBS is being done as a Stage 1 procedure under general anesthesia, patients can take all usual Parkinson medications like normal up to and including the day of surgery.
b) Sinemet (levodopa/carbidopa)and Dopamine agonist—continue through surgery if patient will be taking oral meds. If expected period NPO (greater than or equal to several days) decrease dose by half the week prior to surgery to avoid Parkinsonism Hyperpyrexia Syndrome.
c) If patient is on a transdermal patch for Parkinson’s/dystonia (e.g. Neupro), apply according to schedule to avoid post-op rigidity but apply out of surgical field
MAOB-hold two weeks prior to surgery
Myasthenia Gravis
a) Pyridostigmine-continue as ordered, give day of surgery
9. Rheumatologic Medications
Non-biologic DMARDS
a)Sulfasalazine, azathioprine, mycophenolate (Cellcept), cyclophosphamide—consider holding one week prior to surgery due to neutropenia
b)Methotrexate, hydroxychloroquine, leflunomide—continue through surgery
c)Nonacetylated NSAIDs (i.e. salsalate) have no effect on platelets and can continue through surgery
Biologic DMARDS-Best to discuss with Rheumatology and/or Surgeon for guidance of management in the Perioperative period.
a)Hold for 2-3 half-lives before surgery—restart with wound closure ~ 2 weeks after surgery. Consult with rheumatology if any questions about medication management.
i.TNF Blockers
Etanercept (Enbrel)—t ½ 3.5-5.5d, hold 7-10 days prior to surgery
Apremilast (Otezla)—
Infliximab (Remicade)—t ½ 9.5d, hold 3 weeks prior to surgery
Adalimumab (Humira)—t ½ 10-20d, hold 4 weeks prior to surgery
Certolizumab (Cimzia)—t ½ 14d, hold 4 weeks prior to surgery
Golimumab (Simponi)—t ½ 14d, hold 4 weeks prior to surgery
ii.PDE-4 Inhibitor
Apremilast (Otezla) - t ½ 6-9 hrs, hold 3 days prior and resume when stitches are out
iii.T cell costimulator
Abatacept (Orencia)—t ½ 13d, hold 4 weeks prior to surgery
iv.Interleukins antagonist
Tocilizumab (Actemra)—t ½ 11-13d, hold 3 weeks prior to surgery
Anakinra (Kineret)—t ½ 4-6 hrs, hold 1 day prior to surgery
v.B cell depleting agent and other biological modifiers
Rituximab (Rituxan)—t ½ 18 d, hold 4 weeks prior to surgery
Tofacitinib (Xeljanz)— t ½ 3-8 hrs, hold 5-7 d prior and resume 5-7 d post-op if ok
Belimumab (Benlysta)— t ½ 18.3-19.4 days, hold 3 wks prior to surgery and about 10-14 d after surgery
Alirocumab (Praluent)— t ½ 17-20 days, not immune modulating, do not need to stop for surgery
Secukinumab (Cosentyx)— t ½ 22-31 days, hold 4 wks prior to surgery and about 10-14 d after surgery
Upadacitinib (Rinvoq)- t ½ 8-14hrs, ok to continue through surgery for low-risk procedure (per Dr. Knibbe)
Gout Medications
a) Hold colchicine, allopurinol and probenecid on day of surgery
10. Immunosuppressants for transplant
Continue through surgery
If patient is on an mTOR inhibitor (sirolimus or everolimus), recommend discussion with nephrology prior to surgery as these can cause post-op wound healing issues, seromas and lymphoceles.
11. Hematology/Oncology Medication-Best to discuss IN ADVANCE OF SURGERY with Hematologist and surgeon for guidance during perioperative period.
Palbociclib (Ibrance)-- can cause neutropenia, dosed 3 weeks on/1 week off to allow ANC to recover. May need to be held before surgery and up to 1 week after to allow for healing but needs to be discussed with oncologist MUCH PRIOR to surgery to coordinate
Anastrozole (Arimidex), tamoxifen, letrozole, exemestane (Aromasin)-- hold 1 day prior to surgery and day of surgery due to risk for clotting. Should be held up to 1 week after surgery depending on mobility
12. Parathyroid Hormone Analogs
Teriparatide (Forteo) and other similar osteoporosis agents are ok to continue through surgery.
13. PDE Inhibitors (i.e. sildenafil)
If for ED, hold for 24 hrs prior to surgery. Continue if for pulmonary HTN.
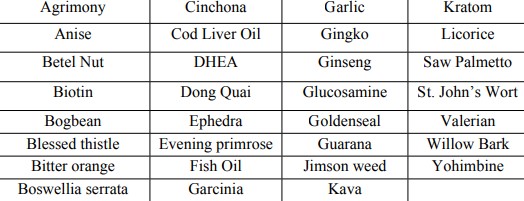
14. Herbal Medications-see table I. CBD oil should also be held for 1 week prior to surgery. Stop ALL herbal supplements for 1 week prior to surgery.
TABLE I
-
Peri-operative Lab/EKG/Imaging recommendations
Ordering Protocol for Labs and Imaging for Perioperative Evaluation
Contributed by Elizabeth Olberding MD FHM FACP, Site Manager St. Luke’s Perioperative clinic
*Sources for recommendations will be cited at the end of the document. These references included evidence based literature, best practice recommendations, expert opinion and advisory council recommendations. The overall consensus recommendation is to use the patient’s history to guide preoperative testing.
Laboratory Evaluation
CBC
Patients with history of anemia
History of recent GI bleeding
Patients with CKD III or greater
Patients undergoing surgeries with possible large blood loss including but not limited to joint surgery or joint revision, intra-abdominal surgery, urology procedures, large neurosurgical procedures including multiple level spinal surgeries, OB-GYN surgeries.
No CBC in the system within one year unless low risk surgery or low risk for anemia
History of cancer on recent chemotherapy
History of liver disease
Interval: Recommend 30-90 days before surgery unless clinical situation has changed
Chemistry-basic
Patients with hypertension
Patients with diabetes
Patients with chronic kidney disease
On digoxin, lithium, seizure medications
Morbid obesity
Older patients > 65 due to risk of CKD
Recent electrolyte abnormality without recheck
ESRD patients and these patients need chem day of surgery also
Interval: Within 30 days of surgery
Chemistry-complete
Patients with liver disease or known abnormality on LFT
Patients with significant alcohol use
Patients on medications with known hepatotoxicity
Coagulation Studies
Only indicated by H and P
Known bleeding disorders
On anticoagulation with warfarin
History of liver disease or abnormal LFT
HgA1C
Diabetics, no A1C within 3 months
Elevated glucose on chemistry
Urinalysis
Major urologic procedures
Should avoid routine preoperative UA unless patient has urinary symptoms. Asymptomatic bacteriuria leads to overuse of antibiotics.
Nasal Swab for MRSA/MSSA
Patients with surgeries with implants or mesh per St. Luke’s policy
EKG
1. Preoperative EKG is reasonable for patients with known CAD, arrhythmia, peripheral arterial disease, and cerebrovascular disease except those undergoing low risk surgery. Level of evidence-B
2. Preoperative resting EKG may be considered for asymptomatic patients without known coronary artery disease except for low risk surgery. Level of evidence-B
3. Routine Preoperative EKG is not useful for asymptomatic patients undergoing low risk surgery. Level of evidence-B
4. The implications of abnormalities on Preop EKG increases with age and risks for CAD. A standard age of risk factor cutoff for the use of preoperative EKG has not been defined. The optimal time interval for an EKG preoperatively has not been determined but within 3 to 6 months is reasonable. (Expert opinion)
5. See attachment on EKG recommendations per ACC/AHA update 2014
Chest X-Ray
Based on clinical situation and patient’s clinical presentation. Should be ordered by physician based on clinical situation and not routinely.
References:
2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Non-Cardiac Surgery. Jour Am Coll Card; Vol 64 No. 22, 2014. 77-127
Practice Advisory for Pre-anesthesia Evaluation: Updated Report by the American Society of Anesthesiologists Task Force on Pre-anesthesia Evaluation. Anesthesiology 2012; 116:522-38.
Pursuit of Abnormal Coagulation Screening Tests Generates Modest Hidden Preoperative Costs. Bushick et al. Journal of General Internal Medicine Vol 4, 1989; 439-497.
Optimal Preoperative Assessment of the Geriatric Surgical Patient: Best Practice Guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society: Chow et al, J Am Coll Surg; Vol 215, No 4. 2012 453-465.
Preoperative evaluation of patients with liver disease. Hanje, James et al. Gastroenterology and Hepatology, May 2007, Vol 4 No 5, 266—276.
Preoperative Evaluation Clinic Visit is Associated with Decreased Risk of In-hospital Postoperative Mortality. Blitz, MD et all. Anesthesiology 2016; 125: 280-94.
Top Ten Myths Regarding the Diagnosis and Treatment of Urinary Tract Infections. Schulz, L et al. The Journal of Emergency Medicine, Vol 51, No 1, pp 25-30 2016.
Update on Perioperative Medicine: Mayo Clinic Meeting. Expert Opinion meeting, Oct 9-11, 2018.
-
Peri-operative Management of Cardiac Implantable Devices
Perioperative Management of Cardiac Implantable Devices:
Pacemakers and Implantable Cardioverter-Defibrillators
Definitions
AICD-Automatic Implantable Cardioverter-Defibrillator
CIED-Cardiac implantable electrical device (global term for devices)
EMI-Electromagnetic interference
ICD-Implantable Cardioverter-Defibrillator
PM-Pacemaker
1. All perioperative patients with CIED (cardiac implantable electrical device) should be identified prior to scheduled procedure and been seen by Pre-admission testing (PAT) or Peri-operative Medicine clinic.
2. All patients with an ICD should be interrogated within 6 months of procedure.
3. All patients with a pacemaker should be interrogated within 1 year of procedure.
4. The following CIED information should be available on day of surgery.
a.Type of device (pacemaker/ICD) and manufacturer
b.Device setting and mode
c.Indication for device implantation
d.Patient’s underlying rhythm and pacemaker dependency
e.Current battery life expectancy
f.Response of device to magnet (pacemakers will pace asynchronously and ICDs will have their tachy (shock) therapy disabled)
5. This information should be obtained by proceduralist team in coordination with the patient’s CIED team (cardiologist) or by referral through the pre-anesthesia clinic (PAT).
6. For emergent procedures, this information can be obtained via patient’s device card or upon examination of a chest x-ray and coordination with device manufacturer. (ICDs will have a much thicker and radiopaque portion of the ICD lead, usually in the RV and near the RA/SVC junction).
7. The anesthesia team will coordinate with the procedure team in developing a plan for reducing exposure to EMI (electromagnetic interference), which may include placement of a removable magnet or CIED reprogramming on day of surgery by CIED team. CIED reprogramming may be required if:
a. Anatomical location of procedure is near device (shoulder, chest, or breast surgery)
b. Patient positioning such that a magnet cannot be used (prone, lateral, severe obesity, etc.)
c. In general, surgery below the umbilicus will not affect a pacemaker or ICD, and rarely is reprogramming necessary, but a magnet should be immediately available.
d. In general, a magnet should be sufficient in surgeries above the umbilicus. The operator is encouraged to utilize brief bursts of monopolar electrocautery (the vast majority of surgical cautery) which would minimize pacemaker inhibition or ICD oversensing.
e. Inactivation of an ICD is recommended for all surgeries above the umbilicus
f. Rendering a PM asynchronous (with a magnet or pre-op reprogramming) is preferable for surgeries or electrocautery above the umbilicus.
g. It is helpful if the ground pad or return electrode for the electrocautery can be placed so that the current would not cross the PM, ICD, or leads and if the current path is kept 6 inches from the PM, ICD, or leads
8. Intraoperatively, patients with CIED will be monitored with continuous ECG with a pacing mode set to recognize pacing stimuli. External defibrillation equipment should be available in procedures where EMI may occur.
9. All patients with ICD’s deactivated should be on continuous cardiac monitor and should have immediate ability of defibrillation until ICD is re-activated.
10. Post-procedural device reprogramming/ interrogation will occur prior to discharge from a cardiac telemetry environment if:
a. Device was reprogrammed to be nonfunctional such as disabling tachycardia detection in ICD or a PM in an asynchronous mode
b. Any intraoperative events suspicious for EMI
c. At the discretion of the procedural or anesthesia teams.
References:
1.Crossley GH et al. The Heart Rhythm Society Expert Consensus Statement on the perioperative management of patient with implantable defibrillators, pacemakers and arrhythmia monitor: Facilities and patient management. Heart Rhythm 8:1114-1154, 2011.
2.Practice advisory for the perioperative management of patients with cardiac implantable electronic devices: pacemakers and implantable cardioverter-defibrillators: an updated report by the American Society of Anesthesiologists task force on perioperative management of patients with cardiac implantable electronic devices. Anesthesiology 114:247-61, 2011.
-
AAB Policy for Lactating Mothers Breastfeeding after Anesthesia
1. It is safe for mothers to resume breastfeeding after anesthesia as soon as they feel ready. There is no need to routinely
“pump-and-dump”.
2. Mothers should “pump” if they do not feel capable of breastfeeding after anesthesia and feel engorged.
3. Postoperatively, almost all short and medium duration PO and IV pain medications are safe for breastfeeding mothers, but may result in the infant sleeping for greater periods.
4. Breastfeeding mothers receiving long acting opioids (Ex; Methadone, Duragesic, oxycodone, etc.), long acting benzodiazepines (Ex; diazepam), or other chronic use pain/anxiety/sedation medication should be followed by a specialized medical team and do not fall under this policy.
5. For mothers that are chronically taking sedatives/narcotics OR for premature infants, breastfeeding recommendations will be on a case by case basis.
Explanation of Policy
• Most of our anesthetic drugs are fat soluble
• The lipid content of the brain >>> Breast Milk >>> plasma
• We indirectly measure the concentration anesthetic drugs in the brain biased on the clinical response (sedation-to- anesthesia).
• When the patient is “awake” the patient has subanesthetic drug concentration in the brain, so breast milk concentration is substantially lower.
• Although lactating tissue is lipid dense, it also has very high blood flow, resulting in drug concentration levels near plasma levels (unlike adipose tissue stores in waist, hips, etc.).
Example;
A lactating mother is administered 10 mg IV morphine and wishes to breastfeed 20 minutes later
D(total dose) = C(milk) * V(milk)
D(total dose) – total dose of drug ingested by baby
C(milk) – concentration of drug in Mother’s breast milk
V(milk) – Volume of milk per feed (~ 40 to 200 ml)
• Weight of patient 50 kg (small woman)
• Weight of Baby 3.5 kg
• Plasma distribution ½ time of morphine = 4.4 min
• Plasma elimination ½ time of morphine = 111 min
• Volume of distribution for morphine = 5.4 L/kg
• EC50 of morphine for post-op analgesia = 0.0015 mg/ml
• Dose of Morphine = 10mg / 60 kg = 0.1666667 mg/kg morphine
• The drug is considered distributed after three plasma distribution ½ times, which is ~ 13 minutes. So the distribution of morphine is complete
• Let’s assume that plasma morphine concentration approximates breast milk concentration (at its short peak, breast tissue may be 1.5 to 2 times greater than plasma)
• Maternal plasma morphine concentration is 0.1666667 mg/kg ÷ 5.4 L/kg = 0.031 mg/ml (D(total dose) = C(milk) * V(milk))
• The baby drinks 200 ml of breast milk which results in an infant PO morphine dose of 0.0062 mg or 0.0018 mg/kg
• The pediatric PO dose of morphine is 0.1 to 0.3 mg/kg (up to 1 mg for our example)
• This subtherapeutic dose is now subject to the baby’s hepatic metabolism (first pass effect)
References
1.Ilett, K.F. Drug distribution in human milk. Australian Prescriber 1997. 20, 35-40
2.Seivers, E., et al. Feeding patterns in breast-fed and formula-fed infants. Annals of Nutrition and Metabolism 2002. 46, 243-248
3.Wittels, B., et al. Postcesarean analgesia with both epidural morphine and intravenous patient controlled analgesia: neurobehavioural outcomes
among nursing neonates. Anesthesia & Analgesia 1997. 85, 600-606
4.Nitsun, M., et al. (2006). Pharmacokinetics of midazolam, propofol, and fentanyl transfer to human breast milk. Clinical pharmacology and
therapeutics, 79(6), 549–57.
5.Chestnut’s Obstetrical Anesthesia 4th edition.
Contributed by Eric Deutsch, MD 8/22/13